"Push and get it out": the dangers of delivering a baby in a country without humanizing childbirth

PINAR DEL RÍO, Cuba— She can't get out of her mind the first sight of her baby after the delivery: her newborn's body had a greyish tone, and he seemed lifeless.
Not long after, she found out that her baby was cyanotic and had almost died for lack of oxygen after a lengthy birth. The medical file describes how doctors tried to resuscitate the baby. The mother remembers her son still covered in blood and fluids, doctors trying to search for a beat in his heart.
She had had an ideal pregnancy, supervised by several doctors. In 39 weeks, the ultrasounds had not shown any anomalies. Also, she had not had gestational diabetes or high blood pressure.
The most likely cause for the cyanosis was a prolonged delivery. The fetus had been exposed to deficient levels of oxygen during birth.
Moreover, the mother, a 22-year-old student of medicine whose identity we are protecting for fear of reprisals, was admitted to the Abel Santamaría Hospital in Pinar del Río (in western Cuba) hoping to give birth to a healthy baby.
But it all started to go wrong the moment she had to go into the pre-delivery room without any of her relatives.
It was a small room, the size of a standard bedroom, without much space to walk. The beds were too close to one another, less than one meter apart, not the best place for her and the other five patients to do their pre-delivery work. They all had to endure the narrow space and their pains.
The doctor who follows her pregnancy from the start, whose identity we are keeping anonymous to avoid government reprisals or losing his job, said that the woman went into labor for 21 hours. Still, the womb's neck would not dilate to the 10 centimeters needed for a natural delivery.
At the time, doctors did not consider performing a cesarean, despite a request for it made by the woman. The hospital's protocols also indicate that for natural birth in women expecting for the first time, the average measure for dilatation is one centimeter per hour. It is a phase that should take up to 12 hours.
The young medical student, exhausted and in pain, had no other option but wait nearly double the time she should have waited for a delivery.
"Hold on and push, I'm not going to take the baby out. You have to give birth by yourself", the gynecologist in charge told her every time she complained of having too much pain.
The expectant mother recalls the effort she made; sweating profusely, she pushed and pushed until his body could not respond anymore.
After a whole day trying to give birth naturally, the doctors found out that the fetus was suffering. Then, they decided to perform an episiotomy, a cut in the area between the vagina and anus, allowing the baby to come out more quickly.
But it was already too late.
"I was always conscious, and at first sight of my baby, I knew he wasn't right," the young mother said. "Then the neonatologist that assisted him told me there was a possibility that he would not survive, that he could die anytime from a cardiac arrest."
According to the 2018 National Health Survey, up until 2017, Cuba had a high rate of cesareans. Nearly 30 percent of births occurred in this way.
There were several reasons why there were so many cesareans performed as opposed to natural births. One of them was the economic incentive attached to cesareans. It was common for doctors to ask expectant mothers for "cash under the table" to do this type of surgery.
But many cesareans were also a direct consequence of a health system that has not yet introduced the concept of humanizing childbirth, which is common in other countries. It is a practice that helps mothers to give birth the natural way by following specific protocols.
One of the measures involves making sure a relative is always there to accompany the mother during the birthing process. The use of painkillers, a large and wide enough space to walk while in the pre-delivery phase, and allowing the mother to have an active role in the decisions regarding the birth, are also part of the guidelines for humanizing childbirth.
Since three years ago, however, it is more complicated for doctors to prescribe a cesarean because the Cuban authorities introduced the so-called Robson Protocol, a standardized system of classification to reduce the number of cesareans performed in the world.
Cuba's objective was to get as close as possible to the rate the World Health Organization considers to be ideal: 10 to 15 percent cesareans.
Gynecologist Laura Tabares, from Havana's Ramon González Coro Hospital, explains that a cesarean is a surgical procedure. As such, it entails risks of postpartum hemorrhages and reactions to anesthesia, and strokes.
On the contrary, natural birth is a physiological process with a much faster and safer recovery. The specialist also explains that a cesarean involves the risk of complications in the short, medium, and long term. These complications include bleeding (three times more than in a natural delivery) or adverse reactions to anesthesia.
"On top of that, after the cesarean, women experience more difficulties in recovering. They need to go the toilet after they have eaten, so they need a liquid diet or food in puree", Tabares said.
She adds that patients also experience difficulties walking, their abdominal wall is compromised, and they tend to lose sensibility around the surgical wound area.
Despite the advantages of natural deliveries compared to cesareans, the introduction of an official policy to reduce the number of these types of operations has given way to situations like the one experienced by the medical student we have been referring to.
Women who needed a cesarean did not have it on time, and their newborns are now suffering the consequences for life.
Official statistics reveal that in Cuba, the number of children who died of birth-related causes increased between 2017 and 2018. The infant mortality rate for babies seven days old or less was 12.9, the worst since 2009.
But the statistics concerning the mortality rate does not take into account cases such as this young mother's, whose baby was born with cyanosis. Although he survived, he now suffers from a type of irreversible cerebral paralysis.
Negotiating a child's birth
For a long time, it was common practice for doctors and expectant mothers to plan a cesarean. The gynecologists benefitted from either money or gifts they received in exchange for performing these surgeries.
In Havana, the country's capital, a cesarean price tends to be higher than in the rest of the island. The fees vary between 50 and 150 CUC (same equivalence to the US dollar).
The baby cannot walk, move his arms, or follow objects with his eyes. The possibility of living a normal life was taken away from him at birth.
The salaries earned by medical specialists in Cuba range from 1,600 to 1,800 Cuban pesos (US$64.00 to US$72.00), including shifts.
Planning cesareans allowed doctors to treat these operations as predictable events with a predetermined schedule. For many women, especially those facing possible complications during labor, the prospect of a cesarean gave them some degree of calmness and peace of mind.
For decades, the number of births that ended up as cesareans multiplied in Cuba. Between 1970 and 2011, the number of cesareans performed went up to 30 percent from a mere 4 percent.
According to the Annual Health Survey, the increase accelerated between 2004 and 2011, with an estimated annual growth of one percent. In subsequent years, the average rate was 30.5 percent.
Another young woman who requested anonymity, also a first-time mother, said doctors promised her a cesarean to give birth to her first child. A microbiologist living in Consolación del Sur's municipality, she had to travel 25 kilometers each way from Pinar del Rio to see her doctor. Every time, she would take a bag filled with presents as partial payment for the agreed cesarean.
"During the pregnancy, I gave presents all the time to everyone in the medical team that followed my case," the 29-year old mother said. "Presents included cards to recharge mobile phones, perfumes, clothes, meat. My husband and I wanted to be very generous because at stake was my safety and my baby's".
The couple's concern was not unfounded. Even though the pregnancy progressed without any alterations and the fetus was healthy, the specialist in charge of her ultrasound scans told her that its size exceeded those required for a natural birth and that the best course of action would be to perform a surgical operation. But when the time came to give birth, in January 2018, things didn't go the way they had expected.
By then, Cuba had already radically changed its protocols regulating cesareans after introducing the Robson classification system in 2017. The country had managed to reduce the number of cesareans (30.5 percent of all deliveries ended in cesareans) to a historical level of 18.3 percent.
At the hospital where the two women were taken, the final decision about performing a cesarean is not made by the gynecologist but the maternity ward director.
The cesarean agreed between the young microbiologist and her doctor never happened, despite all the considerations previously made regarding her baby's size and vaginal cavity dimensions.
The young mother says the doctor who had received all those presents as partial payment for performing a cesarean did not show up at the hospital, as agreed. He never answered any of the calls made by her relatives. He knew beforehand that the cesarean would not be carried out.
The woman had to endure 22 hours of painful contractions. The doctor who followed her pregnancy said that the fetus was already suffering during these longs hours, but the specialists refused to intervene and chose to go with a natural birth option.
Without her consent, doctors cut the woman's perineum, in a procedure known as an episiotomy. She explains the incision reached to the muscle. Then, doctors made a five-point suture on both superficial and deep tissues.
It may seem a brief and straightforward procedure, but afterward, the stitched wound hurts.
"The stitching is very uncomfortable, especially during breastfeeding," the young woman says. "If you make any physical effort, it can open up again. It can happen even while on the toilet. You have to bear with a burning sensation in that area. Also, there is a lot of itching, but you cannot scratch. Doctors think of this as a routine procedure, but for women, episiotomy does not end the day we give birth".
After the episiotomy, her baby showed signs of severe depression. She recalls that he didn't cry until a few minutes after birth.
For the first year, birth's after-effects have impacted the child's life and family. The mother says he cannot grab objects, walk, laugh, or communicate in any way as other children of the same age do.
At the Institute of Neurology in Havana, the child was diagnosed with West Syndrome, an irreversible illness – a type of epilepsy – that causes seizures and severe developmental delays.
The family doctor who follows the case says that "due to medical malpractice at the time of his birth, the child will never be able to talk and walk."

From one extreme to the other
Reducing the number of cesareans was the desired outcome. Still, several of the specialists interviewed for this report said that in applying new protocols, the country's health authorities have gone from one extreme to the other, from allowing multiple cesareans to perform very few or none altogether.
"We are not allowed to do surgical operations on pregnant women," a gynecologist who preferred to remain anonymous told us. "If we risk it and decide to operate on pregnant women, then we are threatened with administrative sanctions. Some colleagues have already been sanctioned because of this".
"The protocols tie our hands", the specialist explains. "We have gone from doing endless cesareans to none. We disagree with this policy, and in our daily practice, we see that such a meticulous control has not been good for the patients. But, going against the rules means risking our jobs".
Another gynecologist from the same hospital in western Cuba explains what the health authorities aim for when enforcing such strict rules is to stop the covert payments in exchange for surgeries – in some cases, unnecessary– and reduce costs in the context of a low economy. Natural birth is cheaper than surgical intervention.
According to data from the Ministry of Public Health, in 2015, each cesarean cost four times more than a natural delivery. "To perform cesarean free of charge in a public health system was unsustainable," the doctor from the Abel Santa María said.
In a country like Cuba, where the practice of humanizing childbirth is not yet implemented, the drastic reduction in the number of cesareans has unpredictable adverse effects.
Several specialists interviewed agree that the forced reduction of this type of operations could put the lives of pregnant and their babies at risk, something that is already happening.
A gynecologist working in western Cuba and who preferred to remain anonymous commented that "since these measures have been implemented, the number of babies suffering from asphyxia, cerebral palsy, fetal hypoxia and, in some cases, even death, has increased."
Official statistics back up the gynecologist's theory. Between 2017 and 2018, several of the leading indicators related to maternal-child health worsened, according to information published in the 2018 Annual Health Survey.
More mothers died during childbirth or the puerperium, the period just after giving birth. In only one year, the mortality rate went from 45 women per 100,000 births to 52, representing an increase of 15 percent.
Also, more children died in the same period. This trend towards increased infant mortality rates continued in 2019. The year closed with a rise of more than 26 percent compared to 3,96 percent in 2018.
Humanizing childbirth (not happening)
Cuba has the lowest infant mortality rates compared with most of its neighboring countries. The island's health indicators are very similar to those in Europe.
But unlike some countries that have been improving their provisions for childbirth care, focusing on the welfare of women and promoting natural deliveries, the Cuban health system is still lagging behind this trend.
A study published in the Cuban Magazine of Public Health reveals that medical facilities' structural problems in Cuba prevent hospitals from providing a humanized service for childbirths.
But the shortcomings of implementing the concept of humanizing childbirth are caused not only by the economic difficulties the country is facing, which in turn undermines the possibility of having more private spaces, equipment to measure babies' heart rate, and access to medication.
It is also due to a lack of training for the medical staff. Several of the gynecologists interviewed for this report, some of them recent university graduates, don't even know what humanizing childbirth is because it was not part of the curriculum. As a result, obstetric violence is seen as usual, and it is not considered a problem.
In June 2019, during the XVII Congress of the Cuban Society of Obstetrics and Gynecology, this type of gender violence was then recognized as a problem.
In the event, Cuba acknowledged that delivery rooms in the country's hospitals do not comply with several of the practices and protocols stipulated for humanizing childbirths.
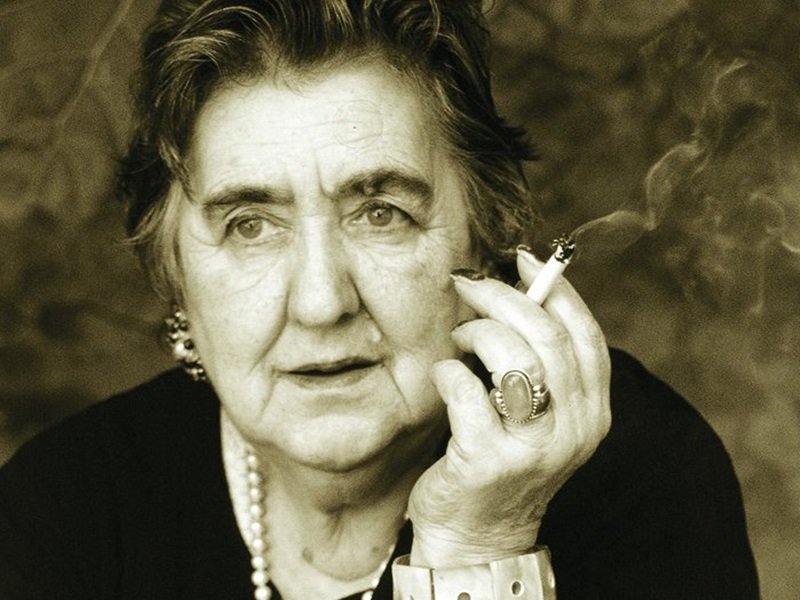
Thais Brandao, a Brazilian psychologist and researcher on obstetric violence, explains that this is a broad concept recognized by some international monitoring centers as the most invisible form of violence against women.
"To not let women about to give birth to be accompanied by someone they trust - a woman's right as recognized by the WHO - is obstetric violence," Brandao says. "To not let pregnant women walk during the pre-delivery phase or choose a position they feel more comfortable with during birth, is also violence."
Brandao adds that the use of forceps, the Kristeller's maneuver (an extinct practice consisting of pressing down the woman's abdomen during the final stages of birth to aid a vaginal delivery), an episiotomy as a routine procedure, and denying a cesarean when needed are all considered obstetric violence.
In Cuba, women often have to go through childbirth independently and share a very narrow space with other patients. These women are subjected to frequent pelvic exams by more than one person, with no privacy at all.
They don't get to decide anything during childbirth and are often not provided with information or asked for their consent, for example, to use forceps. The curettage of the uterine canal goes ahead without anesthesia.
"We don't have protocols in place for humanizing childbirths," doctor Laura Tabares says. "We don't do them due to lack of resources and infrastructure."
Expectant mothers in Cuba do not get anything to help bear the pain during childbirth. It is not common to supply any alternatives to painkillers such as massages, birthing balls, breathing techniques, relaxation, or epidural anesthetic.
Medication is only used in "selected" cases. Four of the doctors interviewed said that access to this product is very restricted, and often it is used in patients with strong links with the government or hospital managers.
Verónica Márquez, also a first-time mother, was not lucky enough to be among those "selected" cases. At 27, she checked into the hospital last September. She was already 40 weeks into her pregnancy but did not have any signs of giving birth. So, doctors had to induce labor with an oxytocin infusion.
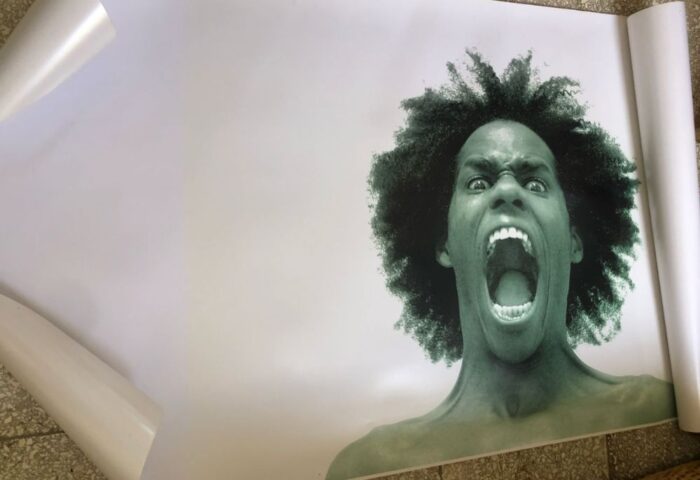
"They took me to the pre-delivery room with other patients that had been there for many hours already, bearing the pain," she says. "When you are surrounded by other women you don't know, and some are yelling because they cannot give birth, then you feel even more nervous and traumatized. I dreaded thinking that it could also happen to me".
Márquez remembers that after the induction, she started to have contractions, one after the other. "I felt as I was being ripped from the inside," she says. "The pain was such that I threw up seven times."
During that time, even though the room was full of medical staff, no one came to see her.
"I kept biting my hand because I didn't know what to do to lessen the pain," the young mother recalls. "The doctors just made fun of me, and they didn't do anything to help me."
Once in the delivery room, Verónica was accompanied by two medical doctors. They performed an episiotomy on her.
"They asked me to push," she recalls. "And then they climbed onto the birth table, one at each side and started pressing down the abdomen by the sides of my ribs. They got my baby daughter out at 6.15 pm. They pulled her out using forceps while pressing my abdomen down. I know forceps can be dangerous; they didn't warn me of the risk before; they didn't tell they were going to cut me either".
Doctors described the birth in the medical history as "hard, traumatic, and with the use of medical equipment." For four months after the procedure, Marquez had to go to the pathology consultation because there has been a partial tearing of the uterus during the intervention.
"I felt as if I was at the butchers. After that experience and if I have to go through it again, I don't think I would be capable of having another child."
"In Cuba's health institutions, there is a very patriarchal and chauvinistic model," Brandao says. "Health practitioners tend to objectify women's bodies when it comes to treating them".
The specialist believes it is vital to train the health personnel at a medical level and the concepts of gender violence and humanizing childbirth.
Many Cuban women remember when they gave birth to their children, especially the first one, as a traumatic event. They had little information or control over it.
The young medical student remembers when her child was born. He has now been diagnosed with an irreversible cerebral palsy and is living in a vegetative state.
"Since my boy was born, I haven't stopped thinking that if I had received a different treatment back then, my reality now would be different. We have been stripped of our right to live a normal life".
This young woman is a single mother. Her boyfriend abandoned her when he found out about the child's condition. Thanks to her family's help, she has been able to continue with her medical studies.
Contributors to this report: Maykel González González, and another journalist who wishes to remain anonymous because she is under surveillance by Cuba´s Security apparatus.
This report is the result of a workshop on in-depth journalism, organized by the Institute of War and Peace Reporting IWPR, an organization whose mission is to contribute to the creation of peace and democracy by creating the conditions conducive to peace and democracy through a free press. In collaboration with local media in countries where freedom of the press is still incipient, IWRP provides practical training to journalists.
▶ Vuela con nosotras
Nuestro proyecto, incluyendo el Observatorio de Género de Alas Tensas (OGAT), y contenidos como este, son el resultado del esfuerzo de muchas personas. Trabajamos de manera independiente en la búsqueda de la verdad, por la igualdad y la justicia social, por la denuncia y la prevención contra toda forma de violencia de género y otras opresiones. Todos nuestros contenidos son de acceso libre y gratuito en Internet. Necesitamos apoyo para poder continuar. Ayúdanos a mantener el vuelo, colabora con una pequeña donación haciendo clic aquí.
(Para cualquier propuesta, sugerencia u otro tipo de colaboración, escríbenos a: contacto@alastensas.com)
















Responder